Belgium stands at the forefront of personalised cancer care in Europe. With robust infrastructure and strategic initiatives in both health data sharing and molecular diagnostics, the country exemplifies how health systems can evolve to meet the demands of precision oncology. However, key challenges such as reimbursement and workforce shortages remain. Below, we explore two critical factsheets that shed light on Belgium’s efforts and gaps in revolutionising cancer care through data and diagnostics.
Quick access
Explore Belgium’s commitment to advancing personalised cancer care through two focused factsheets. One outlines the national approach to health data infrastructure and genomic data sharing, while the other examines molecular diagnostics, including the implementation of NGS and challenges around reimbursement and standardisation.
Click below to access each document directly.
Revolutionising Health Data Uptake
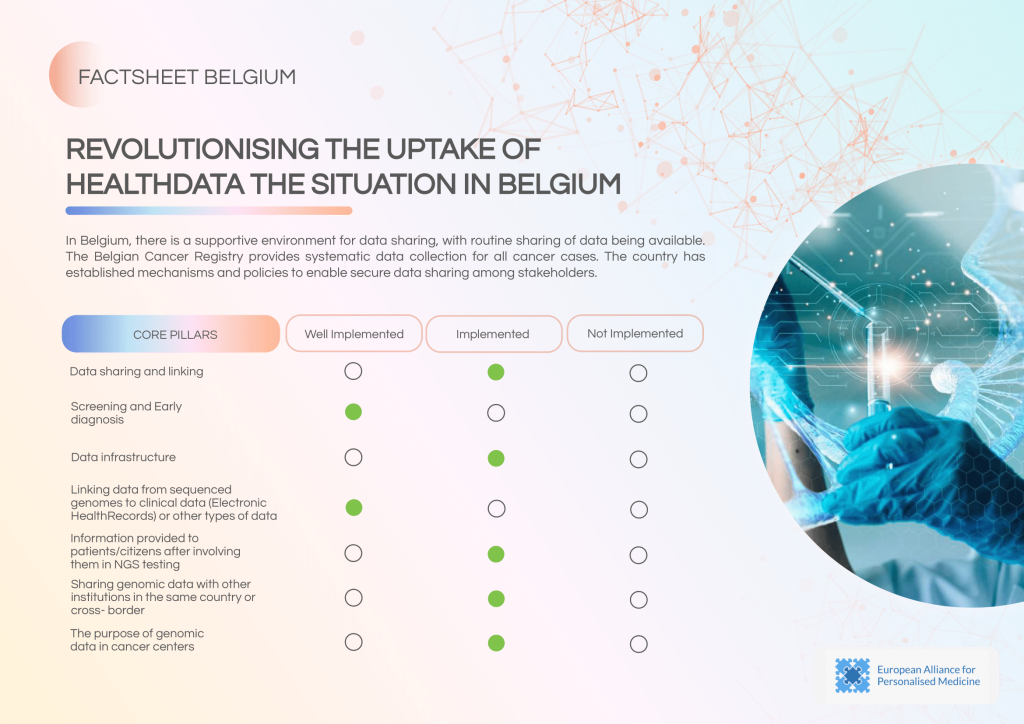
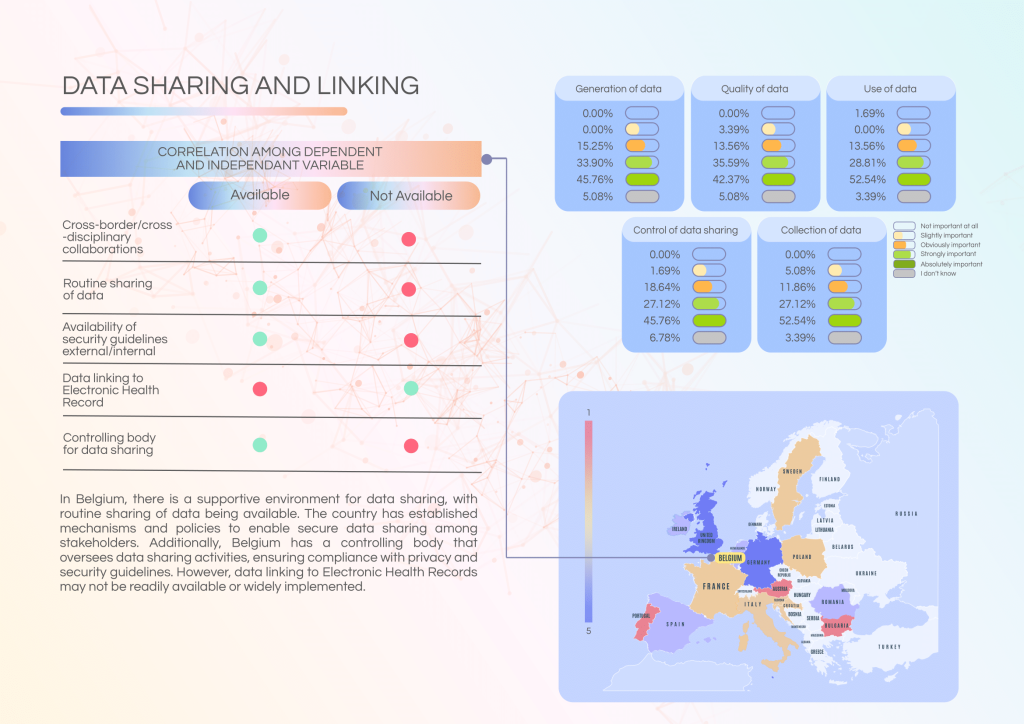
Belgium has built a structured framework for the secure and routine sharing of health data, underpinned by a national Cancer Registry and a designated regulatory body. However, data linkage with Electronic Health Records (EHRs) and standardised communication with patients post-genomic testing remain underdeveloped, creating missed opportunities in real-time decision-making and personalised care.
Current strengths of the system include:
- Active Cancer Registry collecting and maintaining comprehensive national cancer data.
- Clearly defined security protocols and a controlling body for data sharing governance.
- Routine data sharing within the country, especially among major cancer centres.
Key gaps and challenges:
- Limited linkage between genomic data and EHRs prevents broader clinical integration.
- Inconsistent data-sharing practices across institutions and regions.
- Patient engagement and delivery of NGS-related information vary widely by centre.
Priority actions to move forward:
- Mandate genomic-EHR integration to enhance clinical relevance of shared data.
- Standardise cross-centre data-sharing protocols for national consistency.
- Improve patient communication strategies post-testing to meet health literacy needs.
Revolutionising Molecular Diagnostics
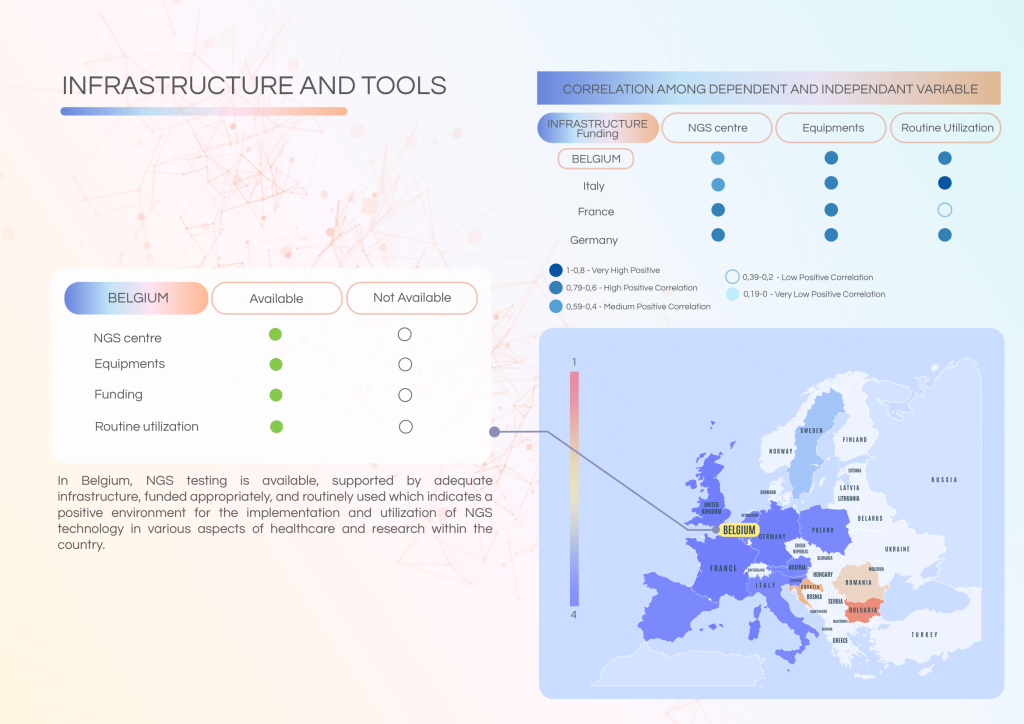
Belgium is among the European countries with a relatively advanced uptake of Next-Generation Sequencing (NGS) technology in cancer care. Infrastructure is well established and NGS is routinely used in clinical practice. However, challenges related to reimbursement, education, governance, and workforce capacity continue to affect equitable access and national scalability.
Key strengths of the Belgian system include:
- A robust NGS infrastructure, including well-equipped centres and regular utilisation of molecular diagnostics in patient management.
- Active Molecular Tumour Boards (MTBs) that support multidisciplinary review and personalised treatment planning.
- High levels of understanding and awareness of NGS among stakeholders in larger institutions.
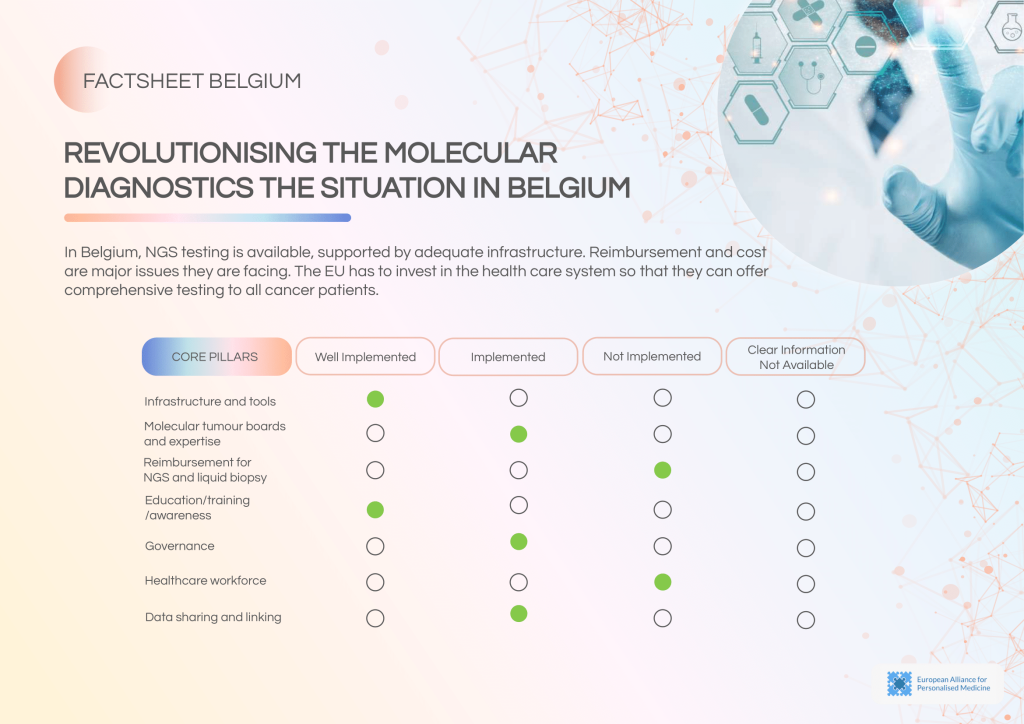
Persistent barriers and gaps:
- Reimbursement delays for NGS and liquid biopsies limit access, particularly outside of academic centres.
- Inconsistent access to training and education, especially outside major urban centres, leaves some professionals underprepared to interpret or use NGS results.
- Gaps in governance, including insufficient external quality assessments and uneven adoption of international standards, pose risks to testing reliability.
- A shortage of qualified healthcare professionals impacts diagnostic turnaround times and integration of precision oncology.
Policy actions required:
- Introduce dedicated reimbursement pathways for comprehensive genomic testing.
- Scale up national training programmes on genomics and personalised cancer care.
- Enforce external quality assurance protocols across all NGS labs.
- Invest in recruitment and retention of oncology and molecular diagnostics professionals.